KRH Grappling with High Patient Volumes, Strained Staff
Hospital has so far managed operations without eliminating services; KRH officials ask public to help “stop the surge” of COVID-19
By Myers Reece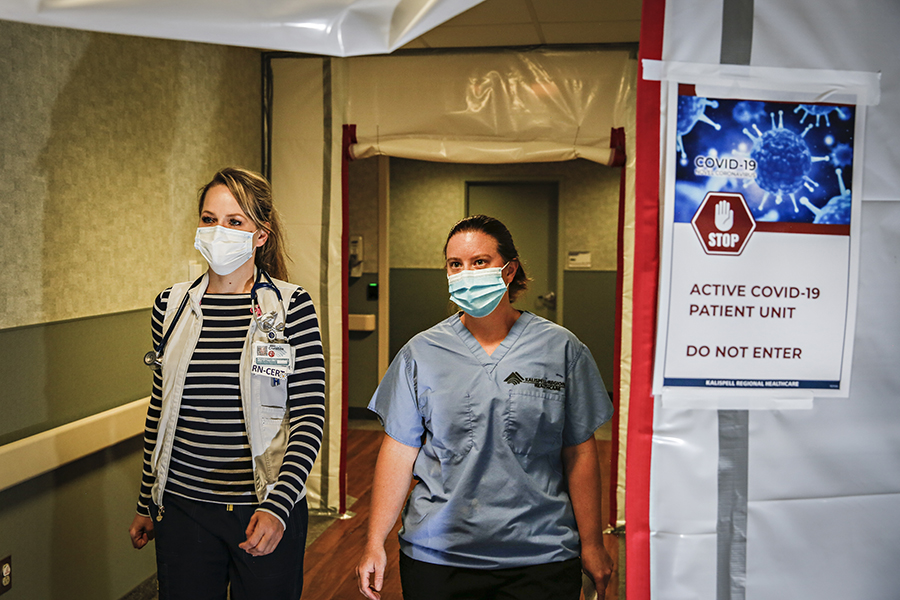
Kalispell Regional Healthcare officials say the local health care system has been dealing with high patient volumes and strained staff, exacerbated by an influx of COVID-19 patients in addition to a steady stream of non-coronavirus patients.
In response to the prolonged recent spike in local cases, the hospital is seeking to amplify its community outreach message of “stop the surge” by encouraging committed adherence to health precautions and pointing the public to its COVID-19 resource page at www.krh.org/covid-19, which is regularly updated.
Dr. Cory Short, a Kalispell Regional Medical Center (KRMC) hospitalist and acute-care physician executive, said the metric he tracks is capacity of the combined 125 adult acute-care beds at KRMC and the HealthCenter. Recently, 80% to 90% of those beds have been occupied, at times drifting into the high 90% range. On Oct. 23, the occupancy rate was 83%.
“The consistency that we’re seeing the 80s to 90s across all seven days is different than historical perspectives,” Short said on Oct. 23.
In the first Montana Department of Public Health and Human Services (DPHHS) hospital capacity report released Oct. 8, KRH was under 70% of capacity overall. That number had dropped to 49% in the Oct. 22 report, although occupancy rates fluctuate throughout any given day and week, and the state includes more beds in its calculation than in Short’s adult acute-care measurement. The DPHHS report broadly describes “inpatient beds” without categories.
KRH has 354 licensed beds altogether, with the bulk of acute-care beds at KRMC and additional beds of varying types at Pathways Treatment Center, Montana Children’s medical center, Brendan House, HealthCenter and North Valley Hospital.
The hospital has been regularly treating more than 20 hospitalized COVID-19 patients, and at times close to 30, as the virus has spread throughout Flathead County, which consistently has more than 600 active cases, while health officials confirmed three new COVID-19 deaths last week, raising the county’s total to 26. KRMC has a dedicated 12-bed negative-pressure COVID unit and has been using other areas of the facility for COVID patient overflow.
Hospital officials say the high patient volume overall, combined with COVID-related employee absences, is stretching staff thin across a broad range of the workforce: nurses, housekeepers, therapists, physicians.
“The staffing challenge is very real,” Short said, noting that staff shortages are an issue statewide and beyond.
Officials say efforts to address the issue and ensure safe patient care have included employees working extra shifts and bringing in traveling nurses. KRH has also stopped quarantining COVID-exposed staff who remain asymptomatic, which is allowed by Centers for Disease Control and Prevention guidelines for essential health workers.
“That’s very telling for what staffing is going through right now,” Andrea Lueck, a registered nurse at KRH, told Kaiser Health News. “We’re so tight that employees are called off of quarantine.”
Mellody Sharpton, a KRH spokesperson, said hospital workers who are exposed to an infected person are tested within three to five days and monitored for symptoms as they continue working.
Short praised the dedication of supervisors and employees, who he said have done an “incredible” job staffing up when necessary, including coming back into work on off days.
Jeana James, a certified medical-surgical registered nurse and inpatient manager at the HealthCenter, said KRH typically expects higher patient numbers in the summer, followed by a decline in the fall. This year, however, the patient volume has remained “steadily consistent” into autumn, requiring “all hands on deck.”
“We’re grateful for our staff right now,” James said. “They’ve been working really hard.”
From a staffing standpoint, Short said the hospital is dealing with the same COVID-19 issues as other employers, with workers forced to stay home due to a variety of reasons related to positive detections, childcare and quarantines.
“Those things are always popping up,” he said.
Staffing is a major discussion point in ongoing collective-bargaining negotiations between KRH management and unionized nurses, who say staff ratios were a concern long before the pandemic, dating back to a restructuring that went into effect in January 2019, which was a catalyst for the unionization push.
Carol Mitch, a member of the nurses’ bargaining team and a registered nurse who has worked in the KRH system for 17 years, said the restructuring led to higher patient ratios for staff and an exodus of nurses, including many experienced senior nurses, creating an atmosphere that Mitch called “demoralizing.”
“The model itself doesn’t really work well in patient care,” she said. “We’re working to restore the staffing ratios so we can once again provide that exceptional care and retain our employees.”
Mitch added: “Everything has been exacerbated by the pandemic.”
Further complicating the current picture at KRH is the number of patients, both COVID and not, coming from communities across the state: Hamilton, Butte, Anaconda, the Blackfeet Indian Reservation and across the Hi-Line all the way from Glasgow, more than 400 miles away.
“You can never predict who’s going to come from where and when they’re going to come,” Short said.
That dynamic is a natural byproduct of KRH’s efforts to increase its footprint and partnerships across the state.
“A big part of our organizational goal is to be a community partner to the region and the state,” Short said. “COVID has helped to further define that on a statewide level.”
“The silver lining amidst this marathon,” he added, “has been the support that everyone has been offering each other from a statewide standpoint.”
COVID is resource intensive, and takes considerable time and preparation simply to offer baseline care even to patients with less severe cases, which impacts workflow, Short said. Its mere presence, surging or not, adds one more serious disease to the vast constellation of maladies for which KRH is already responsible for treating as the primary health care institution for a large region.
“We never really know what will be coming through the door,” Short said. “We may plan ahead, but on any given day we never know if 10 positive COVID patients or non-COVID patients are going to come through the ER.”
The U.S. Army Corps of Engineers oversaw the construction of an alternate-care facility on the vacant top floor of Montana Children’s in May. If COVID hospitalizations were to spike significantly, KRH could use that facility to accommodate more than 90 non-COVID patients, although staffing concerns would likely grow more urgent.
During an Oct. 15 meeting for the Flathead City-County Health Board, KRH President and CEO Dr. Craig Lambrecht said a shortage of available personnel was stressing the system more than bed availability. Lambrecht made his remarks in support of additional restrictions to stem the tide of surging COVID-19 cases locally, although the board didn’t approve any new measures.
“We’re bringing in traveling nurses because the tax on our staff is going to be something we have to pay attention to. The slope of the curve doesn’t look encouraging,” Lambrecht told the health board. “We’re busy, it’s crazy, the stress on staff is real, and we’re preparing for this for the long haul.”
So far, Short said the hospital has been managing the recent high patient volumes and staffing concerns without eliminating services. He said KRH officials routinely evaluate that possibility and have a “plan to adapt” if necessary.
Short and James stressed the urgency of flattening the curve locally through habits such as mask wearing and social distancing. With greater community buy-in and widespread adherence to those measures, Short said “we would see a dip in the numbers, which in turn would help to decompress the hospitals.”
“As a hospital in general,” James added, “we’ve been trying to speak that same message since March and really push it out into the community to help stop the surge and conserve our workforce.”
KRH officials ask the public to visit the hospital’s COVID-19 webpage, which offers numerous resources, including information about schools, testing, mental health, Q&As with experts, and more.
Visit the website at www.krh.org/covid-19.